It has been a year since I posted and honestly, life has been pretty “unremarkable” (clinical term for nothing going on). To me, boring is good but I realize that this may cause some angst for those who follow my story or for more recently diagnosed patients looking for guidance. In a nutshell, I am doing as well as anyone with stage IV lung cancer could be doing and here are my top 10 highlights from this past year.
10. I celebrated my 10 year wedding anniversary with my beautiful wife, Varisara. We were college sweethearts and I couldn’t imagine anyone else being by my side for all these years. When we said “in sickness and in health”, that was no joke. I’m so grateful to have been able to spend these last 10 years married (and 15+ years) with her, supporting each other and growing together in this crazy journey called life.

9 & 8. One of the biggest things I want to do while I am still able is to travel the world. This year we definitely made that happen, going on 9 trips in the past 12 months. We had smaller trips (weddings in Miami and Ohio to celebrate the Theisses and the Chesrowns), a few long weekends (Atlanta for Spring Break, Chicago because Mommy travels for work alot, the San Francisco Bay area for Atitaya’s 40th, and the Bahamas with the Winkels and Andersons), one major trip to celebrate 10 years together in Paris & London, and two cruises – making a total of 8 cruises together since we started dating. It has been a whirlwind of a year exploring the northern hemisphere. I’m hoping next year we’ll be able to explore a bit further, as Avery gets older.










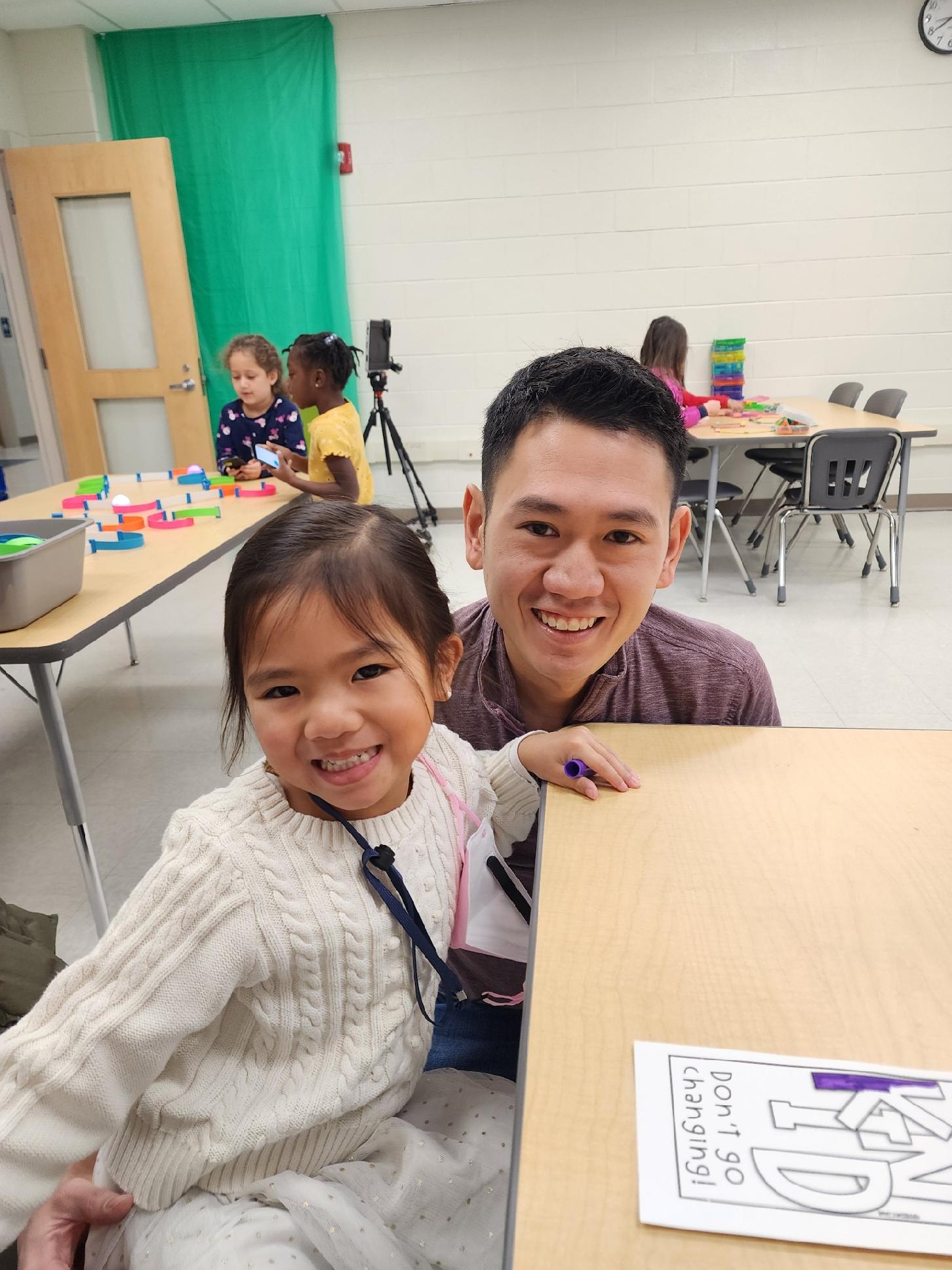
7. Speaking of Avery, I can’t believe I have a 7 year-old daughter. She was just 3 months old when I was first diagnosed and I remember hoping I could make it just a bit longer so I could hear her call me “dada”. Now she calls me “bruh” and plays video games, just like I did when I was younger. Although very sassy (like her mom), she is also very bright and has become insanely curious (like her dad). This year, I thought she was old enough to understand and I finally told her that I had cancer. She had so many questions like “ What is cancer?”, “Why do people get cancer?”, “Is that why you are home more now?”. It has been the joy of my life watching her grow and actually being here to raise her through some of her biggest developmental years, which has maybe resulted in creating a mini female version of myself (oops!).

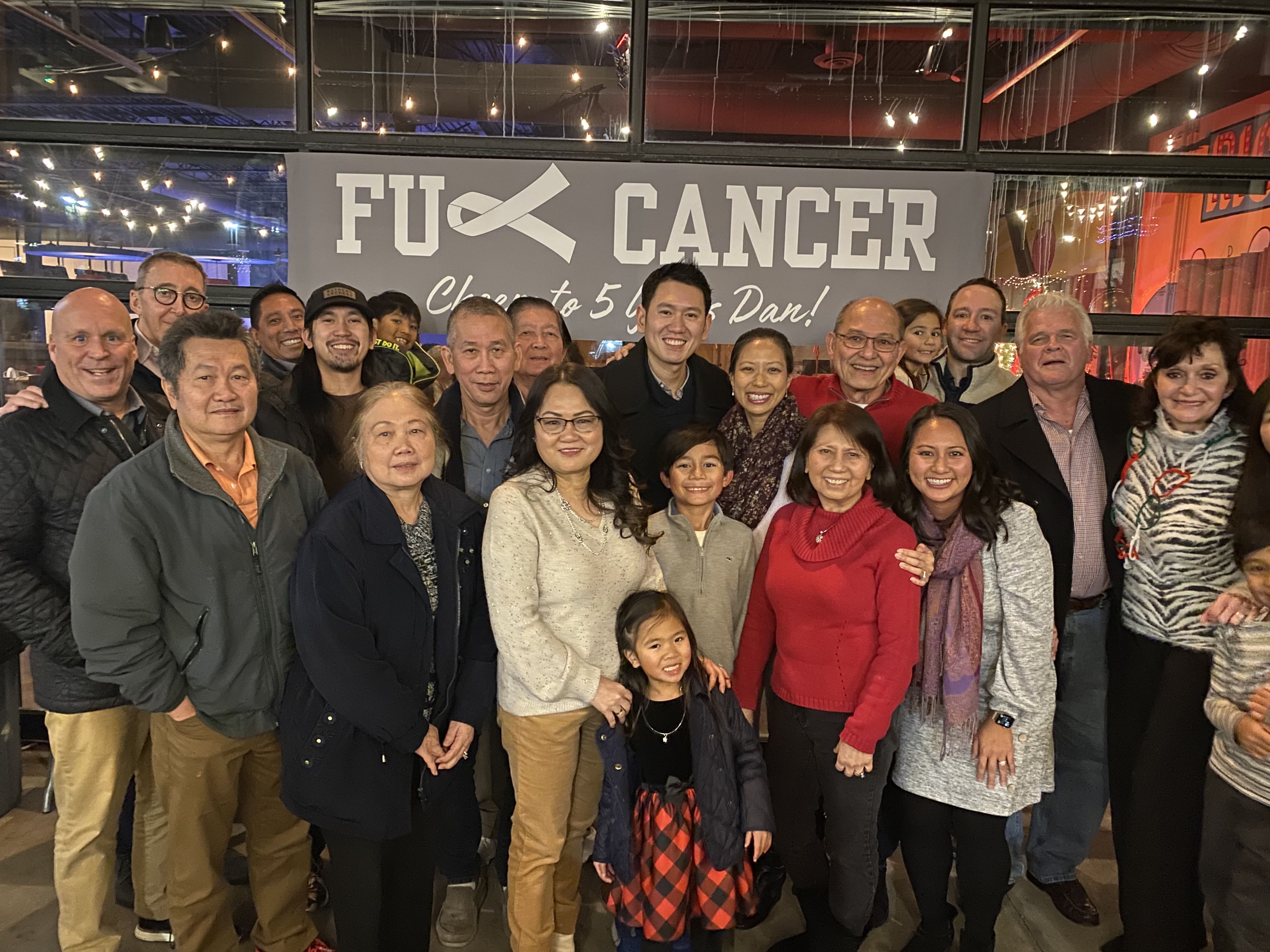
6. I celebrated my 6 year cancerversary in December. It came and went like any normal day and honestly, that’s how I like them. Don’t get me wrong, it is a huge milestone – it marked 6 years from when my perspective on life changed and I focused on the things that really mattered. However, in the grand scheme of things, this is not something I want to shine a spotlight on every year (kind of how I feel about my birthday these days!).
5. Since I get to stay home more these days, I get to spend a lot more time with Avery. This year, she lost her 5th tooth and she pulled them all out herself (am I raising an aspiring oral surgeon?). I also chauffeured her (and sometimes her friends) to 5 different camps this summer, but the best part of the summer was really during the weeks where she wasn’t in camp and we got to have “daddy day care” – we went to the library, freshened up on her math skills, learned loads of new technology (i.e., new video games), and she even helped me with housework.



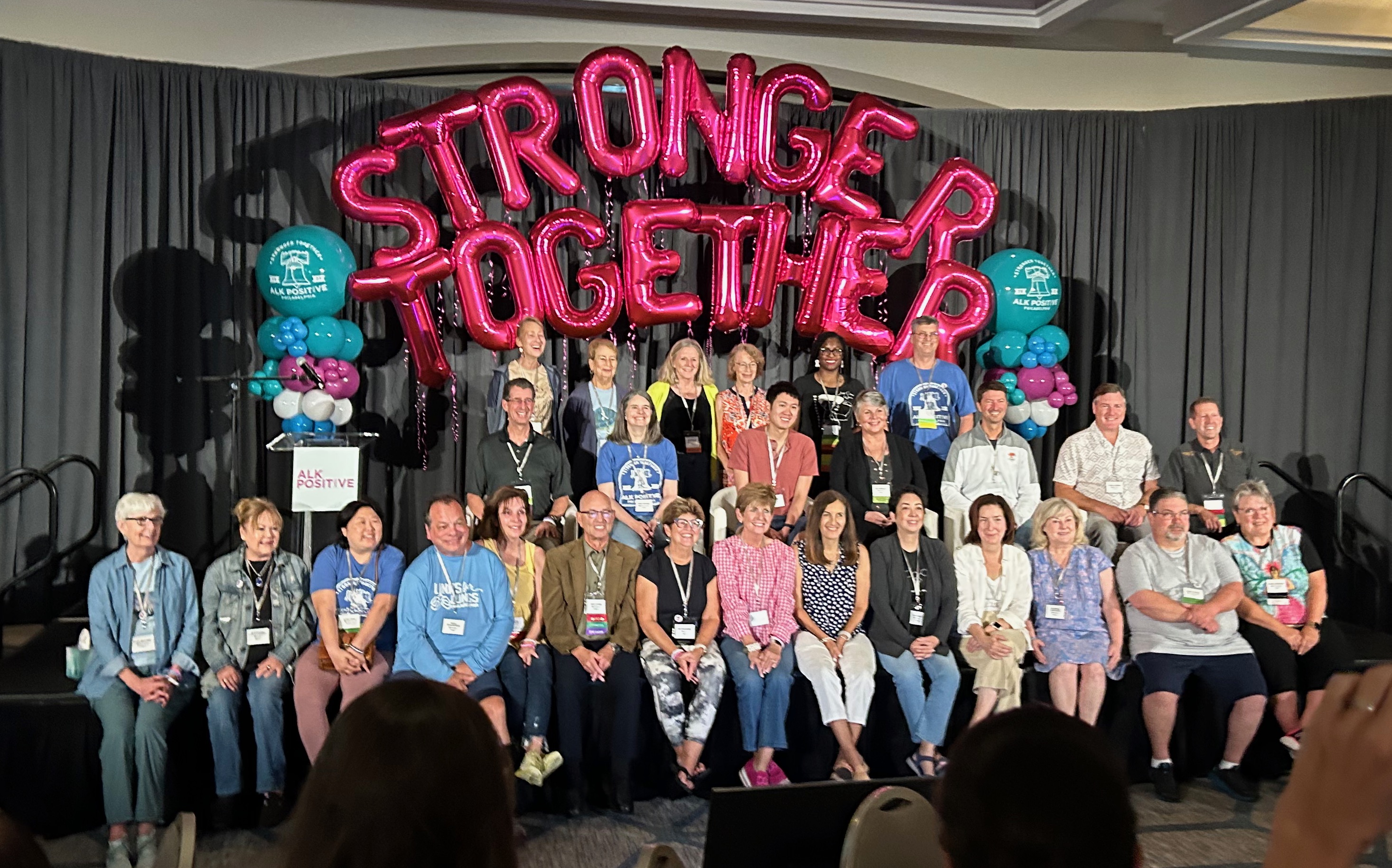
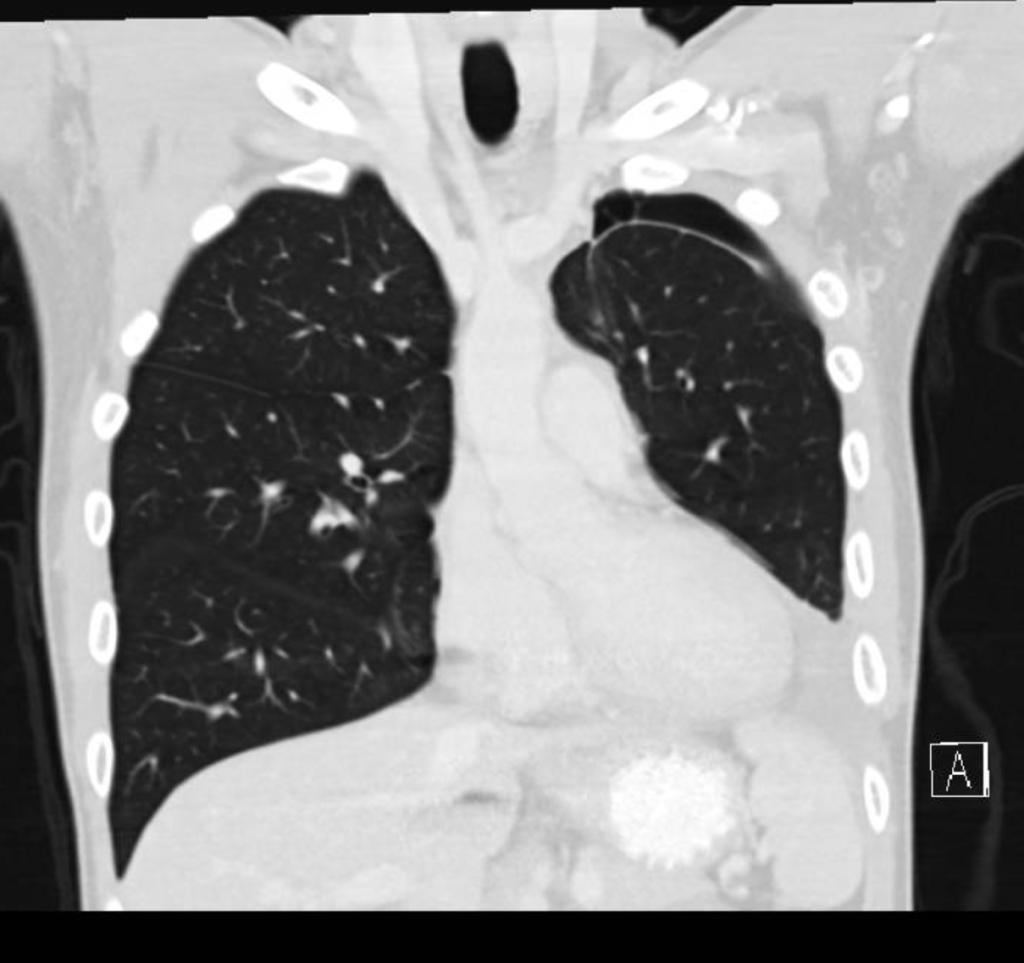
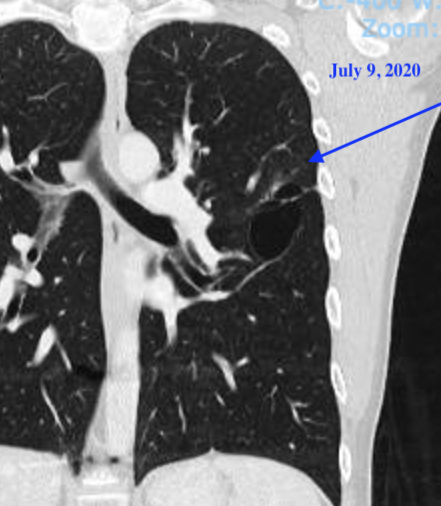
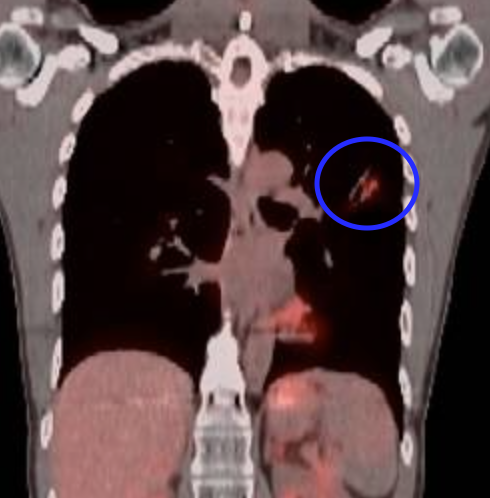
4. Since my last post, I have had 4 scans (all clear!). My oncologist and I started to have the talk – when should we start increasing time between scans? It’s crazy to think that since diagnosis, I have had 80+ scans (am I mutant yet?) and over 40 office visits with my oncology team. I remember in one of the first visits – when I started on the quarterly cadence – Dr. Hall said “I hope you live long enough so I can see you less often”. In case you are unfamiliar, these various scans (CT, MRI, PET) are all fantastic ways to monitor for progression; however, they emit a ton of radiation that accumulates over time and radiation is a known cause of cancer. As a doctor, I can certainly understand wanting to space out scans more because the act of monitoring cancer can actually cause new cancer, but as a patient the scans give me peace of mind that there is nothing to worry about (at least for 3 months at a time).
We are looking to space the visits out to 4 months in between scans, but we are also exploring a potential DNA marker test, which would consist of periodic blood tests to check in between scans. Less radiation, more monitoring – seems like a win to me…if we can pull it off. This is a novel test and we have to find out if my tumor cells have enough DNA to provide a baseline for the monitoring. Unfortunately, the tissue resected from my lobectomy was not able to yield any results. Wish me luck that the last sample collected before that (from my first surgery over 6 years ago) is still available and can provide the genetic material needed.
3 & 2. It has been over 2 years since my lobectomy. Recovery from this surgery is still a new norm that I am trying to get used to. I still get winded going up a flight of stairs, ran the slowest mile of my life (but at least I made it through), and randomly get phantom pains at the surgical site. I constantly have to tell myself to slow down and that I’m not as fit as capable as I used to be. Case and point – I accidentally broke 3 ribs playing pickleball. At my last scan, my doctor asked if I recently had “trauma”. I laughed to myself because I had suspected as much, but the scans actually confirmed it. I am just grateful that I am still able to stay active (although not as active as I used to be) and have one less spot to worry about (the mothership – primary tumor – that I wanted to get removed when I was first diagnosed).
1. I am still on the 1st line medication since my diagnosis, Alectinib. Because I have been able to tolerate the treatment relatively well, I have to awkwardly remind people that I have cancer because on the outside, I look perfectly healthy. The other day, Varisara asked me why I was so tired and I had to remind her that I have increased fatigue due to the Alectinib. I remember getting tired when I was finishing up residency a few years ago and even during my time as an attending, but the effects really wear you down after being on the medication for over 6 years. For those on Alectinib looking to fight the fatigue, I have found that Adderall helps to provide a temporary energy boost. I only take it when there is a real need, but over the years that has shifted from “rarely” to “occasionally”.
All in all, I actually think this has been a pretty remarkable year. I have settled into a new normal where I am granted a reprieve from being sick. I have had the privilege of seeing and experiencing many things that I never thought I would live to see when I was first diagnosed. I have been able to appreciate the things I have and try to live life to the fullest. Here is hoping for another ‘unremarkable’ year (clinically speaking)!