
The days following the surgery consisted of getting fit for my back brace, physical and occupational therapy, and a barrage of doctors and nurses constantly in and out of my room to check on recovery, administer medication, and start planning for next steps. Not only was I recovering from major spine surgery, but I also needed to get started with oncology.
The radiation oncologist arrived the day after the surgery to discuss the plan to take care of the lesions in my spine that the neurosurgeon wasn’t able to get out during surgery. Although the wound needed to heal from the surgery, we wanted to get started with radiation right away to prevent any further growth in the spine. We planned to start the radiation treatments 2 weeks after surgery, however, preparations would be done while I was still in the hospital for recovery.
The medical oncologist also came by to check on me. We knew the tumor was metastatic, but we still were not sure of the source. We could only assume lung because that was where the only other mass was found, but preliminary results were not expected until 2-3 days after surgery. When we finally received the results, they were very vague and actually caused more confusion than clarity. The preliminary results still were unable to confirm the cancer source, but also indicated that a possible gastric source could not be ruled out. Even though the CT scans showed no growths in the GI tract, the medical oncologist ordered a colonoscopy and endoscopy just to be sure everything was clear. I was thrilled. I expected to be discharged on Friday and hoped these new tests didn’t extend my stay in the hospital.
The scopes were scheduled for Friday morning at 11am, which I wasn’t told until 5:50pm Thursday night. I had to be NPO (i.e. nothing by mouth – no food) starting at 6pm and I had not planned accordingly. I was looking forward to warm cookies from Insomnia that evening, but those would have to be put on the back burner in exchange for a lovely clear liquid diet and a 2 gallon container of golytely that I needed to consume by the next morning to clear out my GI tract. They should call it goheavy rather than golytely. If you have not had the pleasure of trying golytely, it tastes like seawater. I finished half the container Thursday night and woke up Friday morning to complete the torture. I finished at 9:20am, proud of myself for getting through it without vomiting and ready for the procedure.
The nurse came in to tell me that my procedure was pushed back to 1:30pm because I did not finish the golytely 2 hours prior to the scheduled start time. I was never told about the 2 hour protocol and I was not happy. Hungry and ready to go home, I was frustrated that I had to wait for an extra 2.5 hours. The scopes came and went, confirming what the CT scan had previously shown; the GI tract was clear.
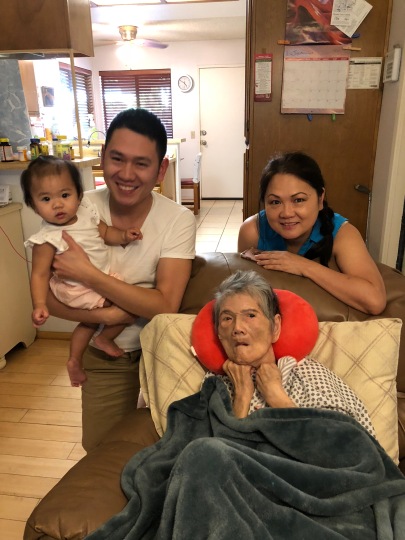
I was finally discharged Friday evening (see picture above), just in time to spend Christmas at home. Final results for pathology were not expected for at least another week.






 Today, I went up to Johns Hopkins University Hospital for a second opinion. My sister-in-law, Atitaya, works with Stand Up 2 Cancer, a non-profit organization that helps to raise funds for cancer research. They work with several cancer research institutions across the country and recommended we visit Johns Hopkins for their work in lung cancer. After talking to the doctor for almost an hour, I left the hospital feeling pretty good. She recommended the same primary treatment as the doctors at UVA and seemed optimistic that the Alectinib was going to work. For now, it seems like we’ll stay the course, but she is also helping to get me plugged in with doctors in Boston who are doing targeted research on ALK mutated lung cancer as well as lung cancer in young non-smokers. This will be beneficial when we need to start thinking about secondary treatment options.
Today, I went up to Johns Hopkins University Hospital for a second opinion. My sister-in-law, Atitaya, works with Stand Up 2 Cancer, a non-profit organization that helps to raise funds for cancer research. They work with several cancer research institutions across the country and recommended we visit Johns Hopkins for their work in lung cancer. After talking to the doctor for almost an hour, I left the hospital feeling pretty good. She recommended the same primary treatment as the doctors at UVA and seemed optimistic that the Alectinib was going to work. For now, it seems like we’ll stay the course, but she is also helping to get me plugged in with doctors in Boston who are doing targeted research on ALK mutated lung cancer as well as lung cancer in young non-smokers. This will be beneficial when we need to start thinking about secondary treatment options.


